
views
“I know one patient who was diagnosed with multidrug-resistant tuberculosis (MDR-TB) and died because she had to wait long for the drug called Bedaquiline. That 24-year-old girl just passed away because she could not get the drug needed for her treatment! It was so shocking for me. Therefore, I decided to challenge this attempt at patenting this drug.”
These are the words of Nandita Venkatesan, a TB survivor herself, who has filed a challenge at Mumbai patent office against pharma company Johnson and Johnson.
Johnson and Johnson, in an application filed at the patent office, wants to extend the patent of the anti-TB drug Bedaquiline. This drug is used to treat TB patients who become resistant to the first line of anti-TB medicines.
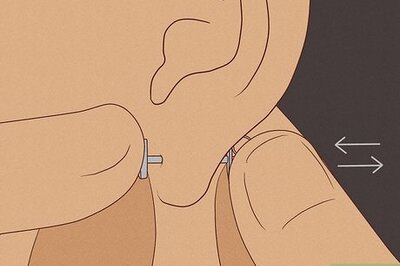
It is extremely difficult to save the lives of drug-resistant patients. Older drugs used for the treatment that are available in the market may cause multiple side-effects like kidney malfunctioning, hearing loss and syndromes of suicidal thoughts. Under such circumstances, Bedaquiline, thus, literally becomes the ‘life-saver’ drug.
The challenge against the patent bid has been filed at a time when the government has announced that another crucial anti-TB drug, Delamanid, will be made available across the country. But experts say that this drug will cover only certain group of patients because it is not referred to all age groups across the states in India.
Nandita, 29, has challenged the patent of Bedaquiline on “technical grounds”, along with another TB survivor, 28-year-old South African Phumeza Tisile.
“It (the salt form of drug) is neither new, nor an invention in law and also under the Indian patent law it is just a new form of an old substance without any change in effectiveness,” says senior advocate Anand Grover, the counsel for Nandita and Phumeza.
Phumeza, who survived XDR-TB, the worst and deadliest form of tuberculosis with chances of survival as low as 20%, spoke to News18 from Cape Town, South Africa.
Phumeza lost her hearing ability to the side-effects of the injectable. She was forced to stop her studies at Cape Peninsula University of Technology for the treatment.
“When I was diagnosed with drug-resistant TB, it was rather shocking to find out that I have to take about 25 tablets a day for two years and an injection every day for six months. Worse part is that the drugs made me sick and the injection made me deaf,” Phumeza said.
“Few years later, after I got cured, I found out that there’s a new drug called Bedaquiline and this drug can replace the injection that causes hearing loss,” she said. “Our task is very simple. Make the drug available to those who need it the most,” she added.
She hopes that the Indian government fixes the patent law.
Nandita and Phumeza both believe it doesn’t make sense that the drug is out of reach for patients who need it as the price is too high.
“I had to undergo long treatment and it (the side-effects of medicines) completely ruined my life… personal and professional,” said Nandita.
She says there is ample proof available that Bedaquilin is safer than many of the injectables that cause hearing loss.
“Even the WHO had given the guidelines last year which say that the usage of Bedaquilin has to increase and (that of) the injections at present given to patients should go down,” Nandita states.
Both these TB survivors had to undergo cochlear implant surgery and can now hear partially in a controlled environment.
Johnson and Johnson got the patent of the base compound of Bedaquiline in 2009 which is set to expire in 2023. The company is now seeking an extension of patent. This move has been challenged by Nandita and Phumeza.
However, the pharma company has committed 10,000 free courses of this drug through USAID. So far, around two-third of this commitment has been delivered.
Nevertheless, this supply cannot fulfill the demand as India has more than 1.47 lakh MDR-TB patients and large section of humanity suffering from the disease remains uncovered.
“The evidence of improved cure rates and lives saved using Bedaquiline is crystal clear,” Dr Anja Reuter, a DR-TB doctor based in South Africa was quoted in the press release of Doctors Without Border.
Doctors Without Border has extended support to Nandita and Phumeza in their legal fight against the patent.
“Bedaquiline is crucial to offering patients a fighting chance without the toxic side effects of drugs that need to be injected. This treatment revolution is already a reality in South Africa, but DR-TB programmes elsewhere need this drug at an affordable price. If this patent application is rejected, generic versions of this drug could be available sooner at reduced prices, saving hundreds of thousands of lives and reducing immense suffering around the world.” Dr Anja was quoted in the press note.
The Indian government has set a target to make India TB-free by 2025. Prime Minister Narendra Modi has said that a TB-free India’s commitment will fulfill the dream of TB-free world.
But, until now, Bedaquiline has been distributed only through donations and the programme is scheduled to end in March this year. The normal course of treatment can cough up as high as Rs 5 to 6 lakh from a patient.
There are no low-price generic drugs available and in such a scenario, the government may have to increase spending manifold to sustain the programme.
MDR-TB is threatening the humanity. In India, there are around 30 lakh TB patients. Experts say that MDR-TB can be deadlier than HIV or Hepatitis. Survival rate is just over 50% but if the patient contracts X-DR TB, which is extremely drug resistance, only 20% patients survive.
The availability of an effective drug for treatment is a big problem. WHO says that in India around 1.3 lakh patients of MDR-TB are added every year. What is more dangerous is that many of these patients remain undiagnosed and they can be deadly carriers of the disease.
















Comments
0 comment