views
- Look for fracture symptoms like instant and acute pain, swelling and/or bruising, trouble bending the finger, or a finger bent at an odd angle.
- If you suspect a broken finger, visit your doctor or an emergency room for a physical examination and X-rays to confirm the diagnosis as soon as possible.
- Ice and compress your finger right away while you travel to the ER. Follow your doctor’s recommendations for splints, pain medications, or potentially surgery.
Signs of a Broken Finger
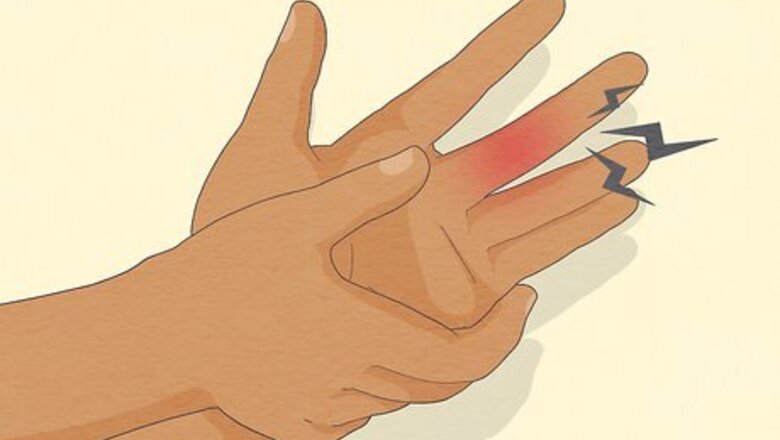
Check for immediate, acute pain and tenderness. The very first sign of a fractured finger bone is pain. The intensity of the pain depends on the severity of the fracture, but it will most likely be focused in one spot near the fracture. Monitor your pain levels after your injury—if they increase, it’s an indication of a break rather than a jam or sprain. It can be hard to identify if you have a finger fracture right away because acute pain and tenderness are also symptoms of dislocations and sprains. If the injury feels more numb or sore than acutely painful, there’s a chance it’s dislocated instead of broken. Look for other symptoms and seek medical attention if you are unsure of the severity of your injury.
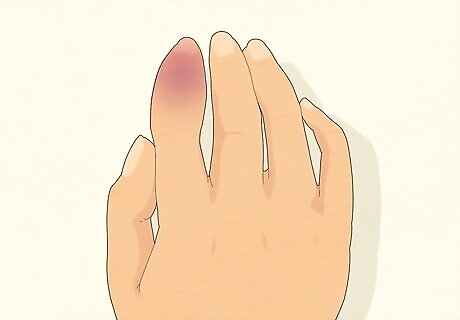
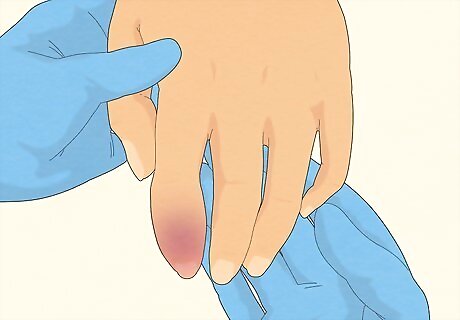
Look for swelling and bruising within a few minutes of injury. After sustaining a fracture to your finger, you’ll notice the acute pain is followed by swelling or bruising at the fracture site. This is part of your body’s natural response to injury—after a fracture, your body activates the inflammatory response which releases fluid into the surrounding tissues. Swelling is often followed by bruising. Bruising happens when the capillaries around the injury swell or burst in response to the increased fluid pressure. The swelling and bruising may not become apparent until you try to move your finger. The swelling may also spread to other fingers or down the palm of the hand. You’ll probably notice swelling and bruising within 5-10 minutes after your first sensations of pain in your finger. If the swelling is minor or the finger doesn’t bruise right away, you may have a sprain instead of a fracture.
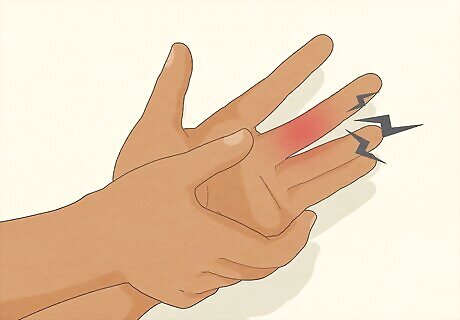
Check if you’ve lost some or all mobility in your injured finger. Try to slowly and gently bend your finger—if it’s painful but you still have your full range of motion, you may only have to treat a jam or a sprain. If it’s painful and you’ve lost range of motion (or can’t move it at all), then a fracture is more likely. Moving a fractured finger is difficult (and painful) since one or more sections of the bone are no longer connected. It’s also likely that swelling and bruising makes your finger too stiff to move comfortably following any injuries.
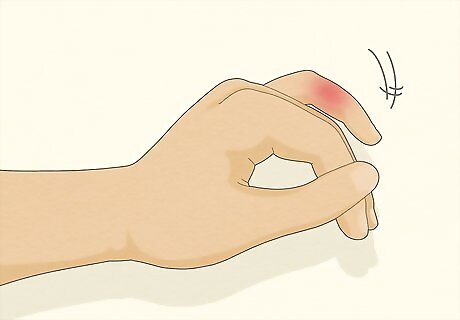
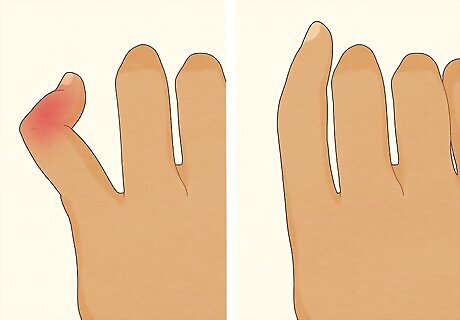
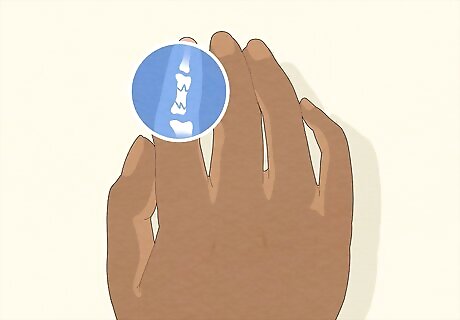
See if your finger bends at an odd angle or if you can see bone. A finger fracture consists of a segment of the bone that is cracked or broken in one or more places. This can lead to deformities like unusual bumps along the finger, a finger that points in the wrong direction, or in severe cases, fingers that seem to bend in the wrong places. If there are signs of bone misalignment, the finger is most likely broken. It may be easier to spot misalignment or twisting on the outer digits like the pinky finger, index finger, or thumb.
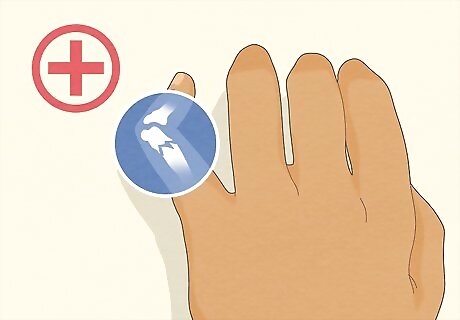
Seek medical attention if you suspect a broken finger. Go to your nearest accident and emergency department if you think you have a finger fracture, especially if the pain and swelling are severe or you see bone through the skin. Fractures are complicated injuries, and you may not be able to tell how severe they are without an X-ray. If you aren't sure whether an injury is a fracture, err on the side of caution and see a doctor. If you have significant pain, swelling, bruising, any deformity, decreased movement of your finger, or visible bone, seek medical attention. Children with finger injuries should always see a doctor. Young and growing bones are more susceptible to injury and complications if they aren't treated properly. If your fracture is not treated by a medical professional, then your finger (and hand) will remain painfully stiff when you try to move your finger. A bone that heals out of proper alignment can cause pain and mobility issues later.
Getting an Official Diagnosis

Get a physical exam at an emergency room or doctor’s office. If you suspect a finger fracture, seek medical attention right away. Your doctor will conduct a physical exam of the finger to evaluate your injury and determine the severity of your fracture. Your doctor will take a note of your finger’s range of motion by asking you to make a fist. They will also look for visual signs, such as swelling, bruising, and bone deformities. Your doctor will also manually examine your finger to look for signs of reduced blood flow to the area and nerve impingement.
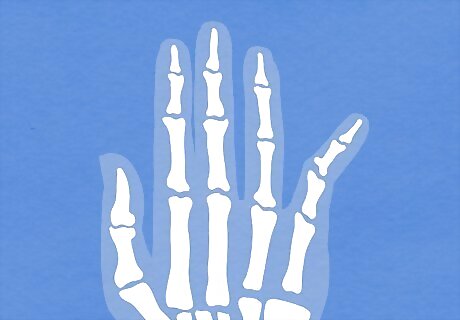
Complete any imaging tests that your doctor orders. If your doctor cannot determine whether you have a fractured finger during a physical exam, they may recommend an imaging test to diagnose the fracture. These might include getting X-rays, a CT scan, or an MRI: X-rays are often the first imaging tests used to diagnose a fracture. Your doctor will place your fractured finger between an X-ray source and an X-ray detector, then send low-level radiation waves through your finger to create the image. This process is completed within a few minutes and is painless. CT (computed tomography) scans are constructed by putting together X-rays that scan different angles of an injury. Your doctor may decide to use a CT to create an image of your fracture if the initial X-ray results are inconclusive or if your doctor suspects there are also soft tissue injuries related to the fracture. An MRI may be needed if your doctor suspects you have a hairline or stress fracture (the kind of fracture from repeated injuries over time). MRIs produce finer details and can help your doctor differentiate between soft tissue injuries and hairline fractures in your finger.
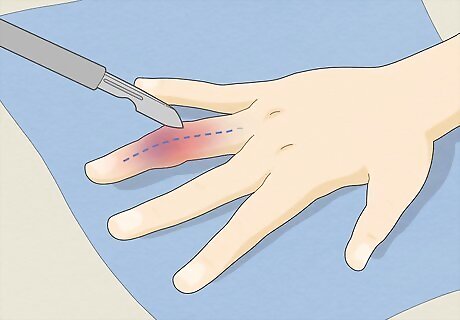
Ask if you need a surgical consultation. Surgical consultations may be required if you have a severe fracture. During the consultation, a surgeon will explain why surgery may be necessary and give an overview of the procedure. Some fractures are unstable and require surgery in order to put bone fragments back into place with aids (such as wires and screws) so that the bone can heal properly. Fractures that seriously hinder mobility and put the hand far out of alignment probably need surgery in order for the finger to regain full movement. Surgery may sound intimidating, but caring for finger fractures is vital. You may be surprised at how difficult it is to execute everyday tasks without full use of all of your fingers!
Treating Broken Fingers

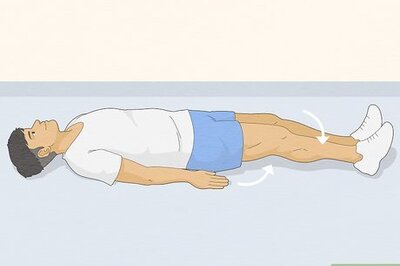
Follow PRICE first aid on your way to the doctor. PRICE stands for protection, rest, ice, compression, and elevation. Apply first aid to your broken finger as soon as possible to manage pain and swelling and to reduce the chances of complications. PRICE is not usually enough to heal a fracture on its own, but it will keep your finger stable on your way to the emergency room or doctor’s office. Protect: Shield your finger from further injury by moving it as little as possible or applying a splint or compression bandage. Rest: Use your broken finger as little as possible to prevent further injury. Do as many tasks with your other hand as you can until you’re cleared by a doctor. Ice: Apply a cold compress or ice pack wrapped in a thin cloth to the finger immediately after injury for 15-20 minutes for pain and swelling. Continue icing as needed for the first 24-48 hours after injury. Compression: Gently but securely wrap your finger with an elastic bandage to manage swelling and immobilize the finger. Ask your doctor if you need to keep your finger wrapped to reduce additional swelling—they may recommend a splint or taping the broken finger to its neighbor (buddy taping). Elevation: Try to rest your hand above the level of your heart as often as possible for 2 days after injury. Try sitting on a couch with your legs over the cushions and your wrist and fingers resting on the back of the couch.
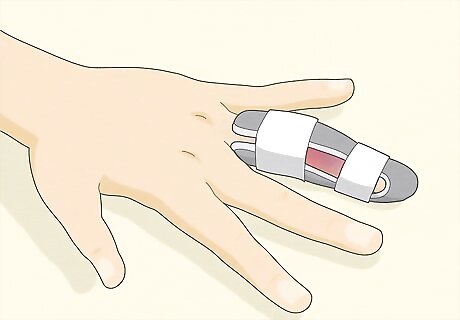
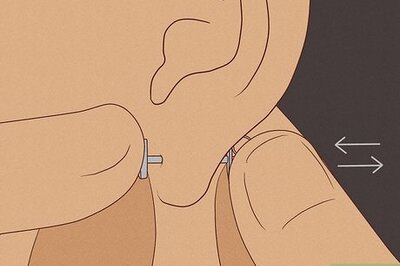
Ask your doctor if you need a splint or other bandaging. Splints are used to immobilize your fractured finger to keep it from developing further damage. Make a temporary splint with a popsicle stick and a loose bandage or loosely tape your broken finger to its neighbor until you make it to the doctor’s office. The kind of splint you need depends on which finger is fractured. Minor fractures may benefit from “buddy taping” (immobilizing the injured finger by taping it to the finger next to it). A dorsal extension-block splint keeps your injured finger from bending backward. A soft splint keeps your injured finger slightly curved toward the palm and is held by soft fastenings. An aluminum U-shaped splint is inflexible and keeps the injured finger from extending. It’s placed on the back of the injured finger to keep it immobile. In severe cases, your doctor may apply an inflexible fiberglass splint that goes from your finger to past your wrist. It's essentially like a mini-cast for your finger.

Take prescribed pain and/or anti-inflammatory medications. Ask your doctor about non-steroidal anti-inflammatory drugs (NSAIDs) or other medication to manage pain associated with a broken finger. NSAIDs work by reducing negative effects of long term inflammation and alleviating pain and pressure put on the nerves and associated tissues. NSAIDs do not inhibit the healing process. Common over-the-counter NSAID medications include ibuprofen (Advil), naproxen sodium (Aleve), and aspirin. Acetaminophen (Tylenol) will also reduce pain, but not inflammation since it is not an NSAID. If needed, take an over-the-counter NSAID like ibuprofen to help reduce pain and swelling before you get to the doctor’s office. Your doctor may also give you a codeine-based prescription medication for the short term if you have major pain. The pain is worst at the beginning of the healing process, and your doctor will reduce your prescription strength as the bone heals.
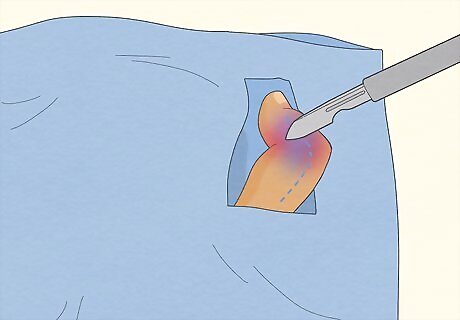
Consider surgery if the fracture won’t heal with splints time. Listen to your doctor’s recommendations and follow through on surgery consultations if needed. Surgery is required to properly treat and heal a fracture when immobilization and time can’t effectively fix it. In general, fractures that require surgery are more complicated than those that only require immobilization. A compound fracture, an unstable fracture, loose bone fragments, and a fracture that compromises a joint all require surgery because the broken pieces need to be guided back into place in order for the bone to heal in the right configuration.
Follow up with your doctor or specialist as directed. Your doctor may instruct you to make a follow-up appointment a few weeks after your initial treatment. The follow-up may include a physical exam or more X-rays to see how your finger is healing. Make sure you keep any follow-up appointments to ensure that you're on the mend. If you have questions about your injury, recovery instructions, or anything else, contact your doctor's office.
Follow your healing guidelines for 3-6 weeks to avoid complications. In general, fractured fingers heal very well after consultation with a doctor and a 4-6 week healing period. The risks for complications following a finger fracture are minimal, but it is still good for you to be aware of them: Joint stiffness may occur as a result of scar tissue forming around the fracture site. This can be addressed with physical therapy to strengthen the finger muscles and reduce the scar tissue. A section of the finger bone may rotate during the healing process, resulting in a bony deformity that may need surgery to help you grasp things properly. The two pieces of the bone may not fuse together properly, resulting in permanent instability within the fracture site. This is known as “nonunion.” Skin infection may occur if there are lacerations to the fracture site and they are not properly cleaned prior to surgery.
Types of Fractures
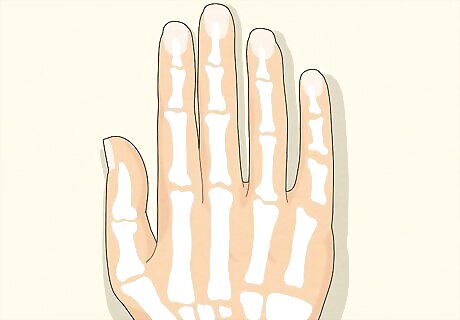
Familiarize yourself with the finger and hand bones to identify fractures. The human hand is made up of 27 bones: 8 in the wrist (carpal bones), 5 in the palm of the hand (metacarpal bones), and sets of phalanges in the fingers (3 in each finger and 2 in your thumb for a total of 14 bones). The proximal phalanges are the longest part of the finger located closest to the palm of the hand. The intermediate (middle) phalanges come next, then the distal phalanges at the tips of the fingers. Acute injuries, such as falls, accidents, and sport injuries, are the most common causes for finger fractures. Your fingertips are one of the most injury-prone areas of your body because they are involved in almost every activity you partake in throughout the day.
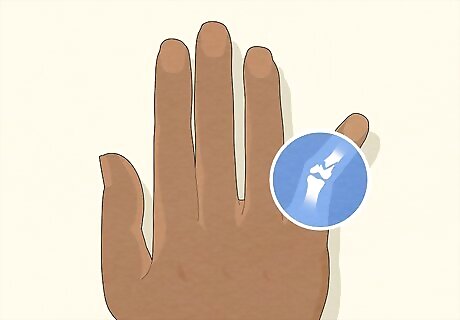
Identify the break as a stable fracture if the bone stays largely in place. Stable fractures are defined by a broken bone with little to no displacement on either side of the break. The bone is broken, but each piece of it is still in the approximate correct place. Also known as a nondisplaced fracture, stable fractures can be difficult to identify because the symptoms can resemble a sprain, bruise, or jam. Stable fractures can usually be healed with only a splint and rest.
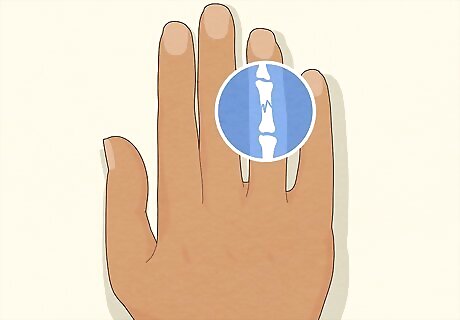
Recognize a displaced fracture when a gap forms between bone fragments. Any broken bone where the two primary sides of the break are no longer touching or aligned is considered a displaced fracture. Since the bone fragments aren’t connected, there’s a possibility your finger will bend or point at a strange angle with a displaced fracture. Displaced fractures are much more likely to require surgery than stable fractures.
Identify a compound fracture by how the bone breaks through the skin. A fracture in which the broken bone has been displaced and a portion of it is showing through the skin is referred to as a compound fracture (also called an open fracture). Because of the severity of the damage to the bone and the surrounding tissue, this injury always requires immediate medical attention. Compound fractures are more likely to lead to infection if they aren’t treated right away and usually take longer to heal than other types of fractures.
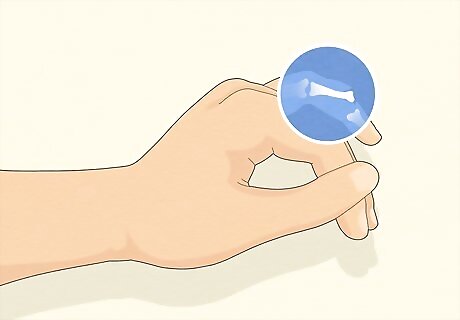
Recognize a comminuted fracture by its multiple points of breakage. This is a displaced fracture in which the bone breaks in at least 2 spots and has shattered into three or more pieces. This is often, but not always, associated with substantial tissue damage. The extreme pain and immobility of the affected finger make it easier to diagnose. Comminuted fractures are common in large and long bones, like in your arms and legs, but can happen in your finger bones since they’re proportionately thin and long.














Comments
0 comment