
views
X
Trustworthy Source
Cleveland Clinic
Educational website from one of the world's leading hospitals
Go to source
As such, the symptoms of aspergillosis start in the respiratory system and then become more widespread with time. Treatment typically involves anti-fungal medications and, in rare cases, surgery.
Recognizing Early Symptoms of Bronchopulmonary Aspergillosis

Take notice of a bloody cough. Aspergillosis starts in the lungs and the tubes (bronchi) that attach to the lungs. The aspergillusspores basically "hatch" there and grow quickly, forming lots of tangled fungus fibers (called fungus balls) within the air spaces. The fungus penetrates the mucus membranes of the lungs and triggers chronic hemoptysis — coughing that brings up blood, sometimes lots of it. In addition to blood, the coughing frequently brings up thick lumps of mucus. Despite the coughing and the spores being able to survive in saliva, aspergillosis is not contagious from person to person. Pulmonary aspergillosis is most likely to develop in people with chronic lung disorders, such as tuberculosis, emphysema, sarcoidosis or even asthma.

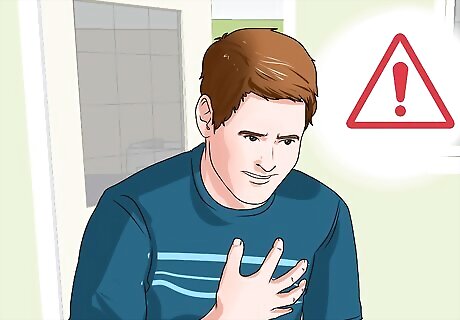
Listen for wheezing and shortness of breath. Along with near constant productive coughing (mucus and blood), the aspergillus fungal infection of the lungs and airways also cause breathing difficulties, such as wheezing and shortness of breath. The breathing is often labored and sounds like a reoccurring mild asthma attack. Without being able to bring in much oxygen with each breath, sufferers constantly appear winded. Cardiovascular exercise is very difficult with pulmonary aspergillosis, so it's best to rest until you get rid of the lung infection. Asthma and aspergillosis often co-exist at the same time. The fungal infection makes the asthma much more difficult to manage with medication. The chronic coughing and shortness of breath can sometimes cause significant chest pain, similar to severe bronchitis or bacterial pneumonia.
Take note of severe fatigue. Another symptom associated with the early stages of aspergillosis is moderate-to-severe fatigue — feeling very tired and run down regardless of the amount of sleep you get. Fatigue is common with most infections, but more so with lung infections because tissues tend to get less oxygen. Due to the chronic coughing, breathing difficulty and potential chest pain, many sufferers of aspergillosis have difficulty sleeping at night and become sleep deprived — which also contributes to the fatigue. In addition to people with chronic lung diseases, chemotherapy patients, organ transplant recipients, people with a very low white blood cell count, people taking high doses of glucocorticoids, and AIDS patients are also more susceptible to aspergillosis.

Watch for unintentional weight loss. Despite not being able to exercise, pulmonary aspergillosis (like most serious infections) typically triggers unintended weight loss. Your immune system burns lots of calories trying to fight the fungal infection, plus your appetite is usually reduced, so weight loss becomes noticeable after a few weeks. Losing more than 5 pounds a week is cause for concern. The coughing up of blood, fatigue and wasting away associated with pulmonary aspergillosis really mimics lung cancer, although survival rates are much better with the fungal infection. Most people lose weight in the face and neck area initially, then the waist, buttocks and thighs. Keep a close eye on your scales if you develop a cough that won't go away.
Be aware of an allergic reaction. Some people with severe asthma or cystic fibrosis have an allergic reaction to the aspergillus mold spores once they breath them in, which is called allergic bronchopulmonary aspergillosis or ABPA. Symptoms are similar to asthma (wheezing and shortness of breath), but can also include stuffiness, a runny nose, temporary loss of smell and headache if the sinuses are involved. An allergic reaction triggers the release of histamine, which quickly causes localized inflammation and congestion. People with cystic fibrosis and asthma tend to have more mucus in their airways, which seems to provide a good environment for the mold to grow in and trigger an allergic reaction. Aspergillosis may also lead to a sinus infection, especially in those with abnormally low levels of white blood cells and those with diabetes mellitus.
Recognizing Advanced Symptoms of Invasive Aspergillosis

Look for fever and chills. As the pulmonary aspergillosis becomes invasive (infects the blood), other more diverse symptoms start to develop, including a fever and chills. A moderate fever with sporadic chills is common for any infection that spreads to the blood, not specific for aspergillosis. Invasive aspergillosis usually develops in people who are already sick from other chronic diseases, so it's difficult to know which symptoms are caused by which condition. A severe fever (greater than 103ºF or 39.4°C) is very rare with aspergillosis — between 99ºF (37.2°C) and 101ºF (38.3°C) is more common.

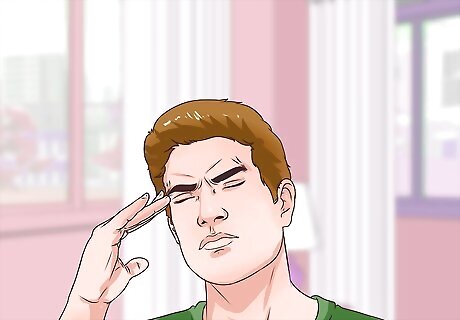
Be alert to headaches and behavioral changes. Once aspergillosis infects the blood, it spreads rapidly around the body, including the brain, heart, kidneys and skin. Telltale signs that aspergillus fungus has infected the brain include headaches and behavioral changes. A person may become quick to anger, get confused easily, seem distracted or appear more obsessive / compulsive. Headaches are caused by mild swelling from the fungal growth. The brain is very sensitive to changes in pressure. Behavioral and mood changes can be triggered by brain swelling, neuron damage/death, reduced neurotransmitter (hormone) production and from any toxins released by the fungi. Symptoms relating to the central nervous symptom are serious and should be addressed by a doctor as soon as possible.

Watch for eye symptoms and facial swelling. Other symptoms that invasive aspergillosis has spread to the brain include eye symptoms (partial or intermittent blindness) and facial swelling, typically only on one side of the face at a time. The fungus can invade the eyeball, but it usually just affects the optic nerve and/or the optical center of the brain. Facial swelling and potential paralysis from aspergillosis can mimic a stroke because it usually just affects one side of the face. Similar to a stroke, fungal damage to one side of the brain affects the opposite side of the face and body. Invasive aspergillosis spreads rapidly and is often fatal, particularly if it gets to the brain or heart, in spite of early treatment.
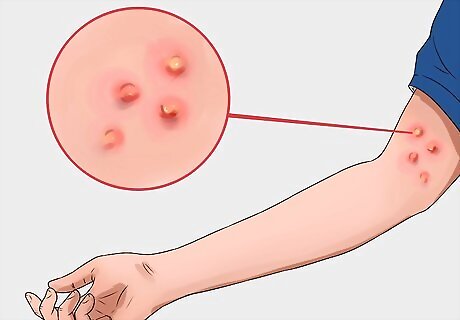
Notice any skin lesions. Although relatively uncommon, aspergillosis can also spread to the skin and cause fungal infections there, particularly in people with very weak immune systems. The lesions or rash appear inflamed and reddish, with a center that's often dark colored (dark blue or black). The fungus can burrow into skin and cause inflammation and itchiness. Skin lesions of some sort occur in about 5-10% of patients with invasive aspergillosis. A skin biopsy (tissue sample) is taken from the lesion before a diagnosis of aspergillosis is made, although many of the above-mentioned symptoms usually occur it spreads to the skin.
Treating Aspergillosis

Wait and observe. In most cases of simple isolated pulmonary aspergillosis, treatment isn't needed as the lung infection doesn't create intolerable symptoms and most medications aren't usually effective against fungus anyways. If the symptoms are only mild or non-existent, aspergillomas is usually closely monitored by chest x-rays every six to 12 months. If your immune system gets stronger, that's usually enough to successfully combat aspergillosis if it hasn't spread into the bloodstream and become systemic and invasive. If the condition progresses, particularly if breathing becomes difficult and significant amounts of blood are coughed up, then corticosteroid and anti-fungal drugs are usually recommended.

Consider oral corticosteroids. Oral corticosteroids (by mouth) are strong anti-inflammatory medications typically recommended for people with aspergillosis who also suffer from pre-existing asthma or cystic fibrosis. Corticosteroids such as prednisone, prednisolone and methylprednisolone are effective for combating allergic reactions and asthma symptoms in the short-term, but aren't used for much more than a few months. Although corticosteroids help prevent allergic reactions and reduce inflammation within the respiratory system, they also suppress the immune system even further, which increases the risk of invasive or system aspergillosis. Other side effects from taking steroids for too long include weight gain, high blood pressure (hypertension) and weakened bones (osteoporosis).

Ask your doctor about antifungal medication. Antifungal drugs are the standard treatment for invasive / systemic aspergillosis, as well as severely symptomatic pulmonary aspergillosis. Your doctor will likely prescribe voriconazole (Vfend), which is preferred because it seems more effective with fewer side effects, or echinocandin. Ask your doctor if antifungals are appropriate for your situation. Antifungal drugs aren't helpful for treating allergic bronchopulmonary aspergillosis, but they can be combined with corticosteroids to improve lung function. If voriconazole isn't effective or well tolerated, other drugs can be tried, such as itraconazole, lipid amphotericin formulations, caspofungin, micafungin or posaconazole. All anti-fungal drugs can lead to serious side effects, including kidney and liver damage, so ask your doctor about the pros and cons of such medications. Antifungal medications are continued until signs and symptoms of the infection are resolved, and may be continued for longer in patients with apparent immune problems.














Comments
0 comment