
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Direct exposure to fungus or mold while bathing (particularly in high risk places such as public swimming pools or gyms) leads to most cases of athlete's foot, but excessive foot sweating combined with poor hygiene are risk factors also. Athlete’s foot initially affects the sole of the foot, in between the toes, but it can spread to various parts of the body if not recognized and appropriately treated.
Recognizing the Common Symptoms

Look between your 3rd, 4th, and 5th toes. These are the most susceptible areas of your foot for fungal infection due to three main factors: they are often neglected when drying the feet; the spaces between toes don't evaporate sweat or moisture very well; they are most prone to abrasion from poorly fitting shoes. If you're itchy in that part of your foot and see some redness, then you might be dealing with a fungal infection. The primary signs and symptoms of athlete's foot include: a scaly, itchy rash that sometimes leads to stinging or burning pain. In advanced cases, inflammation and peeling of the skin occur between the toes — a process called maceration. Athlete's foot is contagious and is easily spread via contaminated floors, towels, socks or flip-flops.

Look for dry, flaky skin on the bottoms and sides of your feet. As athlete's foot worsens it spreads over the sole of the foot, where it causes dry, flaky skin. It will feel rough to the touch and likely be itchy and somewhat irritated. Initially the area will be small, but it will spread and form an irregular margin. There are three main varieties of tinea pedis: moccasin type (involves the sole of the feet), inter-digital type (involves the clefts between the toes) and the blistering type (involves the formation of blisters). Athlete's foot is sometimes called "jungle rot" by members of the armed forces who serve in humid tropical climates.

Be suspicious if you feel itching and burning pain. Foot pain, particularly aches and cramps, are common and usually the result of overuse or ill-fitting shoes, but burning pain accompanied by severe, non-stop itching should make you consider athlete's foot. Fungi cause burning and itching because they burrow into the tissue of the foot and use superficial layers as food. As a result, nerve endings become irritated, which provokes itching and leads to burning pain. Itching is often most intense right after you take off your shoes and socks. Athlete's foot is caused by the same type of fungi that leads to ringworm and jock itch.
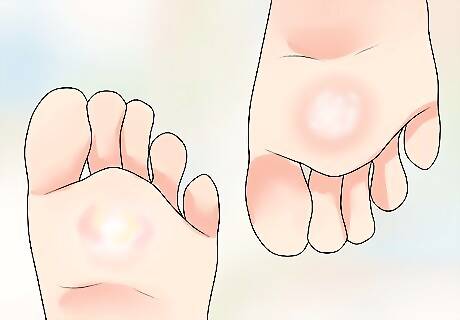
Distinguish between types of blisters. A foot blister can easily be caused by too much walking or running, especially if your shoes don't fit well, but blisters caused by athlete's foot are different — they tend to ooze pus and other fluid and get crusty. Blisters usually form on the thick skin patches, which increases the risk of bacterial infection. After the fungal blisters erupt, lesions with a red, scaly border grow outward and leave a clear center — this is the classic ringworm appearance found over the skin. You're at higher risk of athlete's foot if you are male, frequently wear damp socks or tight-fitting shoes, walk barefoot in public areas and/or have weakened immunity.

Pay attention to toenail changes. The fungus of athlete's foot often spreads to infect the toenails, which then become discolored, thick and even crumbly. In advanced (chronic) stages of infection, toenails become brittle and may even fall off — a condition known as onycholysis. Fungus is difficult to eradicate from nail beds because it burrows deep into the tissue. Burning foot pain and toenail changes are also common with diabetes, so make sure your blood sugar levels are within the normal range.
Confirming Athlete's Foot

See your family doctor. There's no point in guessing about your foot ailment, so make an appointment with your physician and tell him/her your observations and suspicions. In some cases, your doctor may be able to diagnose a fungal infection simply by looking at your foot. However, to confirm the diagnosis (and rule out other conditions), he/she might take a skin sample, add a few drops of potassium hydroxide (KOH) solution and look at it under a microscope. The KOH dissolves skin, but leaves budding fungi intact, making it easy to see. Alternatively, your doctor may view your feet under black light from a Wood's light, which highlights the presence of fungal infections. Your doctor may also do a gram stain to see if there is an underlying bacterial infection. Your doctor may also take a blood test in order to rule out diabetes and other types of infections (bacterial and viral).
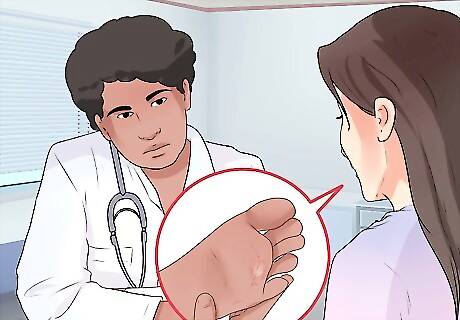
Get a referral to a medical specialist. Medical specialists who deal with skin problems are called dermatologists. A dermatologist is likely to have much more experience than your family physician in dealing with skin conditions, such as infections, rashes and other afflictions. A dermatologist is more likely to be able to do a skin biopsy and KOH preparation under a microscope in their office, so the results can be available in a matter of minutes instead of hours or days. If there is no sign of fungus, then the dermatologist needs to consider other skin conditions that cause a similar appearance such as psoriasis, contact dermatitis, eczema, bacterial infections, gout and venous insufficiency. Psoriasis can be distinguished by its characteristic silvery white scales, which are usually found in the folds of joints.

See a podiatrist. A podiatrist is a foot specialist who also can confirm a diagnosis of athlete's foot and provide treatment. A podiatrist is also a great source of information on what kinds of shoes and socks to wear to prevent fungal infections from reoccurring. Occlusive shoe materials, such as vinyl, rubber and plastic, don't allow for sufficient ventilation, which cause feet to remain warm and moist — providing an excellent opportunity for the fungus to proliferate. Switch to shoes with leather insoles instead. Use cotton socks that absorb water from your feet. Try to avoid socks made with nylon or other synthetic materials. Try to change your socks every day. Wash them in hot water with baking soda to kill any fungus.
Combating Athlete's Foot

Use an over-the-counter anti-fungal preparation. Over-the-counter anti-fungal powders, creams and/or ointments can help rid you of athlete's foot. The topical drugs that are effective against tinea pedis include azoles, allylamines, ciclopirox, tolnaftate, and amorolfine. Keep using the medicine for a couple of weeks after the infection has cleared to prevent its return, as there may be spores buried in the skin. Use the powder to disinfect your shoes and save the cream / ointment for your feet, applying it early in the morning and at bedtime. Fungicidal and fungistatic chemicals used for athlete's foot frequently fail to kill the fungi in the deeper horny layers of the skin, which explains why they're sometimes ineffective.

Try some home remedies. Instead of buying creams from the pharmacy, look in your cupboards for white vinegar (acetic acid). Diluted vinegar (with 75% water) is strong enough to inhibit fungal growth. Soak your feet in diluted vinegar for 10-15 minutes, twice daily, until the itchiness and dryness disappear. Alternatively, soaking your feet in a drying solution of aluminum acetate (Burow's solution or Domeboro solution) can be effective also. Clorox bleach can also be effective for killing fungi and most other pathogens, but it may temporarily irritate your skin and nerve endings. Furthermore, try not to inhale it directly as it may cause dizziness, headache or confusion. Consider an aluminum salt solution, such as aluminum chloride 10% solution or aluminium acetate. These act as antiperspirants by blocking sweat glands. The usual ratio is 1 part solution mixed with 20 parts water (unless a physician instructs otherwise). The solution should be applied to your feet overnight.

Get a prescription for an anti-fungal drug. More advanced or resistant cases of athlete's foot may need an oral (pill) anti-fungal such as terbinafine (Lamisil), itraconazole (Sporanox) or fluconazole (Diflucan). Potent oral medications are reserved for people who don't respond to powders, creams, sprays or ointments. Pills may need to be taken for up to a month or so. Blood tests may be needed before you take these medications to make sure your liver can tolerate them. Treatment for nail fungus may be more intensive and require longer courses (three to four months) of oral medications. Fluconazole 50 mg once daily for 4-6 weeks is adequate to clear most fungal infections. Itraconazole 100 mg once daily for 15 days may be a better alternative.
















Comments
0 comment