
views
X
Trustworthy Source
Centers for Disease Control and Prevention
Main public health institute for the US, run by the Dept. of Health and Human Services
Go to source
While medications can help control asthma, you’ll also need to keep your child away from environmental triggers that aggravate symptoms. With some diligence, you and the pediatrician should be able to control your child's asthma and keep their symptoms in check.
Treating Asthma Attacks

Assess the severity of your child’s symptoms during an attack. If your child can communicate, ask them to describe how bad they’re feeling. Moderate symptoms include chest tightness, wheezing, and coughing. Loud wheezing, difficulty breathing, and trouble speaking are more serious symptoms. If your infant or toddler is too young to communicate, check for audible wheezing and coughing. If they’re very agitated or upset, their symptoms could be serious. Trouble breathing or gasping for air are signs of an emergency.

Call emergency services for severe symptoms. Seek prompt medical care if your child can’t breathe, seems confused, has blue lips or fingernails, or has trouble walking or speaking. Administer quick-relief medications according to the action plan, and call for an ambulance.

Take a reading with a peak flow meter, if you have one. Have your child inhale as deeply as they can and close their lips tightly around the meter’s mouthpiece. They should then blow out as hard and quickly as possible. A peak flow meter is a device that measures air flow from the lungs. Your child should use their peak flow meter when they're not experiencing symptoms to establish their normal range. Compare their score during an attack with their normal range. A score that’s within 80% of their personal best is within normal range. A score between 50% and 79% of their personal best indicates moderate symptoms. Scores below 50% are a medical alert.

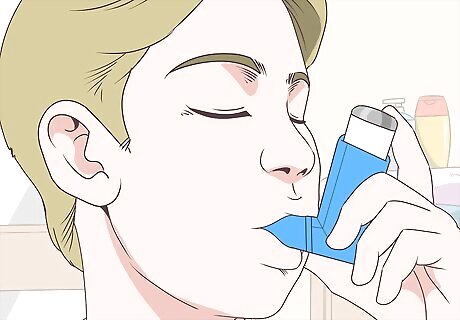
Have them use a short-term bronchodilator, such as albuterol. Help your child use their inhaler according to their prescription. For example, their pediatrician might recommend 2 puffs for moderate chest tightness and 4 puffs for trouble breathing or audible wheezing.
Administer a corticosteroid, if they’re prescribed one. If necessary, have your child take an oral or inhaled steroid according to their prescription. Corticosteroids are often prescribed for severe asthma, especially in children. They reduce inflammation in the airways and can relieve symptoms such as shortness of breath. If your child takes an inhaled corticosteroid, have them gargle after using it to prevent infections. Corticosteroids can slow growth in children, so they’re often only used daily during periods of frequent moderate or severe symptoms. Still, the benefits of controlling asthma outweigh the risk of slowed growth.

Monitor your child's symptoms for 2 to 4 hours. If your child didn’t need emergency care, keep an eye on them for 2 to 4 hours after they use quick-relief medication. During that time, have them use their inhaler as prescribed, such as every 20 to 60 minutes. If their moderate symptoms persist for longer than 4 hours, call their pediatrician. If your child's symptoms become severe despite using quick-relief medication, call emergency services.
Consult the pediatrician if your child has 2 or more attacks per week. When your child’s asthma is well-controlled, they should experience few symptoms. They shouldn’t need quick-relief medicine very often. If they need to use it more than twice a week, ask their doctor to adjust their long-term asthma control medication.
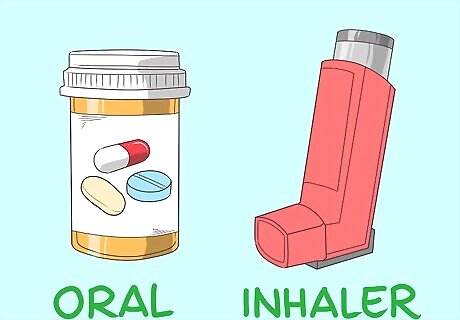
Developing an Asthma Control Plan
Discuss long-term and quick-relief medications with the pediatrician. Your child’s pediatrician will likely prescribe a daily control medication, such as a inhaled long-term bronchodilator. For flare-ups, the pediatrician will also prescribe a short-term medication, such as albuterol. The pediatrician might also prescribe inhaled or oral corticosteroids and medications for allergies. Long-term control medications are taken daily and help prevent asthma flare-ups. Quick-relief medications are used to open the airways during flare-ups. When asthma is well-controlled, your child shouldn't need quick-relief medication more than once or twice a week.
Have your child take daily control medications as directed. Long-term asthma medications are available in pill, liquid, and inhaled forms. Help your child take their asthma control medicine every day, even if they don’t have symptoms. Ask the pediatrician to explain how much medicine to take, when to take it, and how to use the inhaler or nebulizer. Make sure that you read all of the instructions and enclosed pamphlets that come with your child's medication. Your child's treatment plan should thoroughly explain how to administer their medication. Ask your pediatrician or pharmacist if you're in doubt about something.
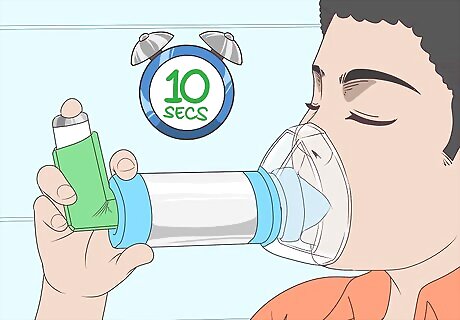
Attach a spacer to their inhaler so it’s easier to use. Children often have trouble using inhalers properly, so ask for a spacer that fits your child’s inhaler. Shake the inhaler, spray 1 to 2 test puffs into the air, attach it to the spacer’s opening, then have your child tightly close their lips around the spacer’s mouthpiece. Press the inhaler to spray 1 puff (or as many as directed), and have your child breathe in slowly and deeply. After they inhale the medication, they can take the spacer out of their mouth. Have them hold their breath for 10 seconds. Then, they should pucker their lips and slowly exhale through their mouth. A spacer collects the medicine, so there’s no need to carefully time breaths with the inhaler sprays. You’ll likely need a prescription for the right spacer from your pediatrician or pharmacist.

Have your child use a nebulizer if they can’t use an inhaler. The pediatrician might prescribe a nebulizer for young children and for some medications. Connect the hose to the machine, and fill the medicine cup with the proper dose. Turn the machine on, and have your child breathe in slowly and deeply through the mouthpiece for 10 to 15 minutes. A nebulizer turns liquid medicine into a mist. Specific instructions vary, so use your product as directed.
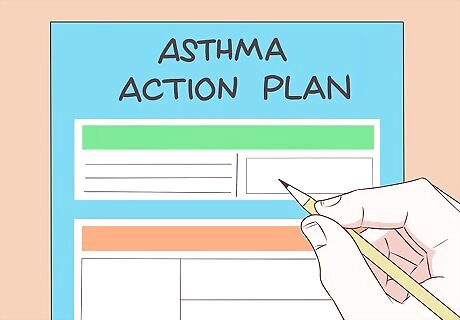
Create a written action plan with your child's pediatrician. Provide your child’s school with a copy. Include information about daily controller medications in the first category. Next, write down what to do if asthma symptoms are moderate. In a third category, provide information about what to do in the event of an emergency. For example, the plan might specify, "If cough and chest tightness are moderate, take 2 puffs of albuterol every 20 minutes. If symptoms don’t improve in 1 hour, take an oral steroid." For severe shortness of breath, an action plan might advise "4 puffs of albuterol, an oral steroid, and calling emergency services if symptoms don’t improve within 15 minutes." The action plan will be posted in the nurse's office with your child's name on it. The pediatrician should sign off on it. In addition to the plan, you should provide the nurse with an extra inhaler and any other medication that your child may require. If your child is old enough, they can also carry an extra inhaler with them, along with a written authorization from the doctor that they are allowed to use it. Consult the pediatrician about what information to include in the action plan. Additionally, see the National Institute of Health’s template action plan at https://www.nhlbi.nih.gov/files/docs/public/lung/asthma_actplan.pdf.
Record your child's normal breathing with a peak flow meter. Have your child inhale deeply and tightly close their lips around their peak flow meter’s mouthpiece. Then, they should blow out as hard and quickly as they can.Image:Treat Asthma in Pediatric Patients Step 13.jpg Have them repeat the steps 3 times, then record the highest score. Their personal best score when they're not experiencing symptoms will provide a comparison during flare-ups.
Eliminating Environmental Triggers
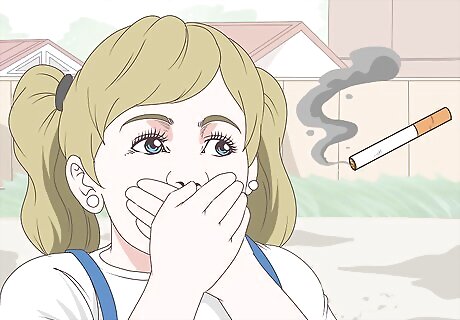
Keep your child away from secondhand smoke. Tobacco smoke is the most important environmental trigger to eliminate. Don’t allow anyone to smoke in your home, car, or around your child. When someone smokes outside, smoke particles still linger on them and can aggravate your child's asthma.

Wash their sheets weekly and use dust-proof mattress covers. Dust and dust mites can aggravate asthma, so change their bed linens weekly. Wash their sheets in hot water, and place a hypoallergenic, dust-free cover over their mattress. You can purchase a dust-proof, allergen-impermeable mattress cover online or at home goods and department stores.

Vacuum and dust your home weekly. While they’re more expensive, vacuum cleaners with HEPA filters are better for people with asthma. They collect fine dust instead of blowing it into the air. If your vacuum doesn’t have a HEPA filter, open the windows when you vacuum to increase ventilation. Additionally, you should regularly dust all surfaces in your home with damp cloth.
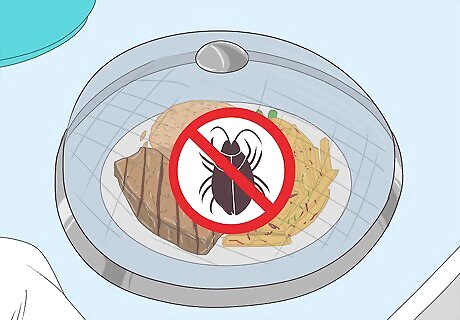
Put food away and clean messes promptly to prevent pests. Insects and mold are triggers, so avoid keeping food uncovered. Don’t let messes stick around and attract pests, and clean the fridge out regularly to prevent mold growth. If you need to deter pests, use baits or traps instead of pesticide sprays.
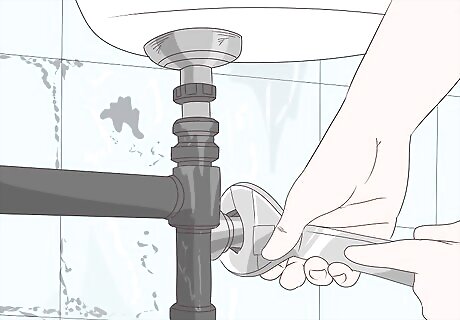
Check for and replace moldy carpets, tiles, walls, or ceilings. If you spot a moldy area, have a plumber find the leakage issue that caused it. Additionally, clean areas that are prone to mold growth at least weekly, such as bathroom tiles and shower curtains. After taking a shower, extend the shower curtain instead of leaving it bunched to prevent mold growth. Using a squeegee or towel to dry the shower area after use is also helpful.

Make sure any pets you own stay out of your child’s bedroom. If you have pets, keep them outside, if possible. At a minimum, keep pets out of your child’s room, and keep the bedroom door closed. If your pet aggravates your child’s symptoms, consult the pediatrician. They might prescribe allergy medication or recommend asking a friend or relative to provide a new home for it.

Get your child tested by an allergist. There are many triggers that can be affecting your child's asthma, such as pollen, exercise, or colds and other viruses. An allergist can determine what these triggers are so that you can limit your child's exposure to them. This could help you better manage your child's asthma. Ask your child's pediatrician for a referral to a specialist.

















Comments
0 comment