views
Can sperm travel through clothing?
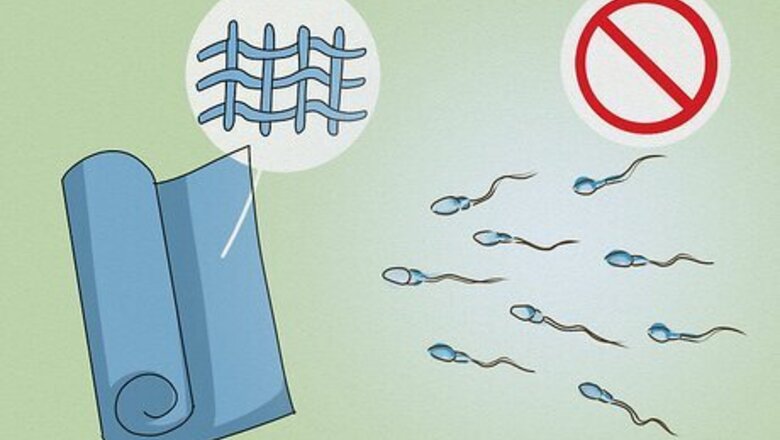
No, it’s unlikely that sperm can go through one or more layers of clothing. Unless the layer of clothing (like a pair of underwear) was completely soaked in semen and was in direct contact with the vagina, it’s unlikely that sperm can go through. However, if the penis penetrated the vagina or semen came into contact with the opening of the vagina (the vulva), pregnancy is possible. Having dry sex (like grinding or humping) with all of your clothes on can’t result in pregnancy. However, pregnancy is possible if you have dry sex without clothes on and semen comes in contact with the vulva or vagina. Wearing or touching clothes with dried semen on them can’t lead to pregnancy. While sperm ejaculated into a condom can survive up to a few hours, sperm on skin or fabric can only survive for a few minutes.
Can you get pregnant from precum?
Possibly, but the chances of getting pregnant from precum are low. The majority of precum, or pre-ejaculate fluid, contains dead sperm or no sperm at all. However, there’s no way to tell when there is or isn’t sperm in precum and you can’t tell when pre-ejaculate is released, which is why the pull-out method isn’t a reliable form of birth control. The pull-out or withdrawal method (in which a guy pulls his penis out of the vagina before he comes) also doesn’t protect you from exposure to Sexually Transmitted Infections (STIs). One study on 27 men found that 11 of them produced precum samples that contained sperm, and 10 of the samples had motile (or moving) sperm. However, there haven’t been enough studies to determine why some pre-ejaculate fluids contain sperm and why some don’t.
Can pregnancy happen from oral or anal sex?

No, you can’t get pregnant from having anal or oral sex. Both the mouth and the anus are completely separate from the genitals. However, oral sex and anal sex can spread the same STIs as vaginal sex. And, pregnancy can happen if semen gets on the vulva or in the vagina. Pregnancy might also be possible if a person ejaculates close to the vagina or if an erect penis comes into contact with the vagina or vulva.
Practicing Safe Sex
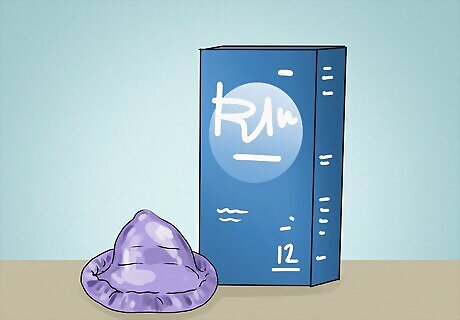
Use condoms or other forms of birth control to prevent pregnancy. Condoms stop sperm from entering the vagina, mouth, or anus, and lessen the chance of getting an STI. Other forms of birth control include birth control pills, IUDs, hormonal implants, vaginal rings, patches, shots, vaginal diaphragms, spermicides, and the morning-after pill. Condoms limit the transfer of body fluids. Choose a male or female condom made of polyurethane or latex and try to carry a couple of them with you at all times. To avoid pregnancy, use condoms from the first moment of genital contact. If you have unprotected sex, talk to your doctor about getting tested for STIs. If you had unprotected penis-in-vagina sex and want to avoid pregnancy, consider taking emergency contraception (the morning-after pill) up to 5 days after the event.
Maintain an open dialogue with your partner(s) about safe sex practices. To avoid confusion or miscommunication with your partner(s), clearly establish what kind of barrier protection (like condoms) and/or birth control methods you want to use, what you’re comfortable and uncomfortable with in the bedroom, and how to get tested for STIs. It’s easier to have safer sex if you come prepared. Make sure you’re meeting up with someone you trust, discuss your expectations before sex, and carry birth control with you. Try to avoid drinking alcohol or using drugs, which can increase the chance you’ll have unsafe sex.

Get tested at least once a year for STIs, even if you have a single partner. If you’re very sexually active or have more than 1 partner, consider getting tested every 3 to 6 months. Suggest to your partner(s) that they should get tested as well to keep all of you safe. In addition, check your body (and your partner’s body) frequently for any signs of sores, rashes, blisters, or discharge. STIs include gonorrhea, chlamydia, syphilis, HPV, genital warts, herpes, HIV, hepatitis (A, B, and C), trichomoniasis, and mycoplasma genitalium.
















Comments
0 comment