views
X
Trustworthy Source
Cleveland Clinic
Educational website from one of the world's leading hospitals
Go to source
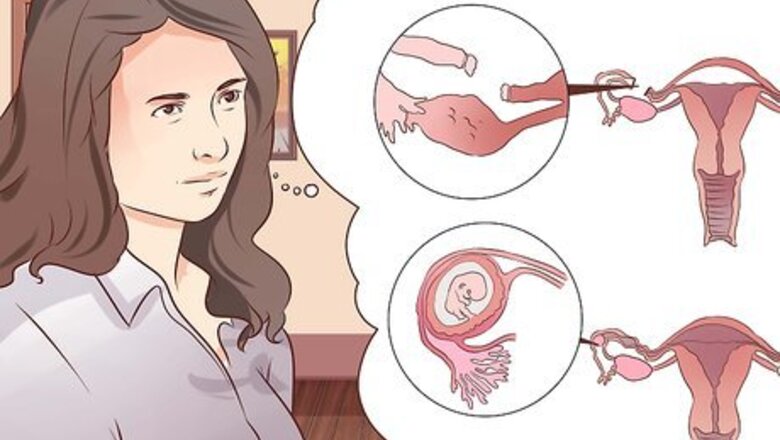
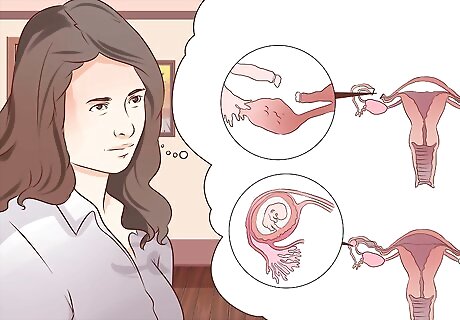
Identifying the Symptoms of Ectopic Pregnancy
Look for the absence of menstruation. If you have missed a menstrual period, and had unprotected sex prior to that, take a pregnancy test. Although an ectopic pregnancy does not occur in the uterus, your body will present with many of the typical signs of pregnancy anyways. If you have an ectopic pregnancy, the pregnancy test would hypothetically always be positive. However, remember that these tests do have the possibility of false positive results or false negative tests, so if in doubt it is always a good idea to visit your doctor for a blood test for a confirmation.
Start looking for other signs of pregnancy. If you are pregnant, whether it has implanted in the uterus (as in normal pregnancy) or in the fallopian tubes or elsewhere (as in ectopic pregnancy), you will still likely experience some if not many of these common symptoms: breast tenderness frequent urination nausea, with or without vomiting absence of menstruation (as previously mentioned).
Feel for any abdominal pain. If you have already confirmed your pregnancy or you still aren’t sure, but you experience abdominal pain, then it could be because of an ectopic pregnancy. The pain mainly occurs due to the pressure exerted by the growing fetus on the surrounding tissue, which in the case of an ectopic pregnancy does not have enough room to accommodate the fetus (the fallopian tubes for instance, the most common site of ectopic pregnancy, are not by any means designed to accommodate a growing baby). The abdominal pain can be sharp and severe, or in some cases there may be no pain. The pain often increases on movement and straining, and is often localized to one side of the abdomen. Shoulder pain can also present due to the presence of blood in the abdomen, which can irritate the nerve that travels up to your shoulder. Know, however, that round ligament pain is very common in pregnancy. This pain, similarly, is located on one side or the other (or both) and can come in intervals (which usually last a few seconds each). The main difference is that round ligament pain tends to occur in the second trimester. The pain from an ectopic pregnancy will usually emerge sooner than that.
Be aware of any vaginal bleeding. Light bleeding may occur due to irritation of the fallopian tubes as they are being stretched, and more profuse and severe bleeding may occur later as the baby grows to the point where the fallopian tubes may actually rupture. Bleeding during any sort of pregnancy is something that warrants examination from your doctor - particularly if it is continual or severe bleeding, in which case you are best to be seen in the emergency department sooner rather than later. Severe bleeding from ruptured fallopian tubes (which can occur as a result of an ectopic pregnancy) can lead to significant blood loss, fainting, and in very rare instances death if not treated promptly by a medical professional. Other serious symptoms (apart and aside from bleeding) which warrant prompt medical attention include severe abdominal pain, lightheadedness, dizziness, sudden paleness, or mental confusion, all of which could indicate a ruptured ectopic pregnancy. Note that something called "implantation bleeding" is entirely normal. This occurs one week prior to your first missed menstrual period (3 weeks after your last menstrual period) and is a pinkish/brownish discharge that should fill more than a few pads. Bleeding from an ectopic pregnancy usually occurs later than this, after the embryo has implanted and begun to grow in a space that cannot accommodate very much growth. However, if bleeding at any time is bright red in color, taking up several pads, and not improving within a day or so, it is important to seek prompt medical attention.
Diagnosing Ectopic Pregnancy
Consider whether any of the risk factors for ectopic pregnancy apply to you. If you are experiencing any of the symptoms mentioned above, you also need to consider if you fall into the high risk group of ectopic pregnancies. Certain factors increase a woman’s likelihood of experiencing an ectopic pregnancy. Generally, women who have had an ectopic pregnancy in the past are more likely to experience such pregnancies in the future too. Other risk factors include: pelvic infections (sexually transmitted infections), multiple sexual partners (as this increases the chance of unknown STI's), fallopian tube tumors or abnormalities, previous abdominal or pelvic surgery, having an IUD, endometriosis, or smoking. Also, if a woman has had "sterilization" (also known a "tubal ligation" surgery, when her "tubes are tied" in an effort to prevent future pregnancy), although this is normally very successful in preventing pregnancy if one were to become pregnant the risk of it being an ectopic pregnancy is notably higher.
Have your β-HCG levels checked in a blood test. This is the first step towards the diagnosis of an ectopic pregnancy. β-HCG is a hormone that is secreted by the developing embryo and placenta, so it rises as the pregnancy progresses and is a more definitive (and reliable) form of pregnancy test. If the β-HCG level is above 1500 IU/L (often between 1500-2000 IU/L is suspicious), but no pregnancy is seen with ultrasound, doctors will worry about you having an ectopic pregnancy. This is because the β-HCG levels are normally higher in ectopic pregnancy than in normal intrauterine pregnancies, so it is certainly a cause for suspicion. If an ectopic pregnancy is suspected due to your β-HCG levels, your doctor will follow this up with a transvaginal ultrasound to see if she can visualize a pregnancy, and its location.

Undergo a transvaginal ultrasound. These ultrasounds can detect 75-85% of ectopic pregnancies (the growing fetus will be able to be seen on ultrasound in that percentage of cases, which confirms its location). Note that a negative ultrasound does not rule out an ectopic pregnancy. A positive ultrasound (one that confirms the presence of a pregnancy in the fallopian tubes or elsewhere outside the uterus), however, is enough to make the diagnosis. If the ultrasound is negative (i.e. inconclusive), but the β-HCG level is high and your symptoms are enough to concern your doctor that you may have an ectopic pregnancy, your doctor will likely recommend a "diagnostic laparoscopy," which is a simple surgery with very small incisions where they can insert cameras into your abdomen to have a clearer look.
Allow your doctor to perform a diagnostic laparoscopy. If your blood tests and ultrasounds seem inconclusive, and an ectopic pregnancy is still suspected, your doctor may perform a diagnostic laparoscopy to visualize your pelvic and abdominal organs internally to look for the spot of implantation. This procedure usually lasts for 30 minutes to an hour.
Treating Ectopic Pregnancy
Seek treatment promptly. Once the diagnosis of ectopic pregnancy is confirmed, your doctor will want to treat you very quickly. This is because the treatment for ectopic pregnancy is much simpler when done sooner rather than later. Also, it is impossible for an ectopic tubal pregnancy to "survive"; in other words, the fetus won't be able to live anyway, so removing the pregnancy sooner rather than later prevents complications (which, if left too long, may become life-threatening).

Take medication that will abort the pregnancy. The most commonly administer medication in this scenario is methotrexate. It is given via intramuscular injection, one or more times, depending upon how much is needed to successfully get rid of the ectopic pregnancy. After the injection of methotrexate is given, you will receive repeat blood tests to check your β-HCG level. If it drops to near zero (undetectable in the blood test), the treatment will be deemed successful; if not, you will receive more methotrexate injections until this goal is reached, and if it still not attained you may need surgery.
Have surgery to remove the ectopic pregnancy. During surgery, your doctors may also repair or remove the damaged fallopian tube if needed. Indications for surgery include: Severe blood loss requiring urgent treatment. Failure of methotrexate treatment.


















Comments
0 comment